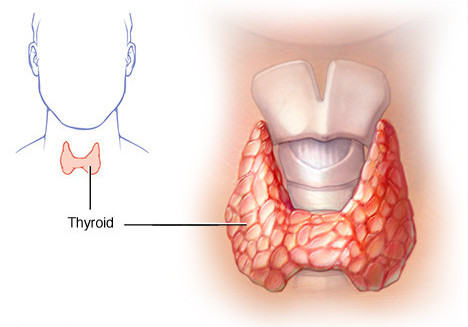
Hypothyroidism results from deficient production of thyroid hormone by the thyroid gland. Since the thyroid hormones regulate metabolism in every cell of the body, a deficiency can affect virtually all body functions. Deficiency of thyroid hormones can result from lack of stimulation by the pituitary gland, defective hormone synthesis or impaired cellular conversion of T4 to T3. No matter what the cause, symptoms such as low energy, fatigue, cold hands and feet, muscle pain, depression and cognitive deficits are common.
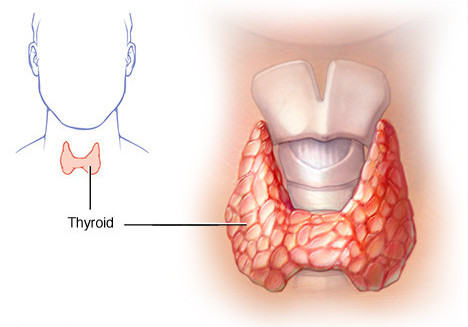
Primary hypothyroidism is caused by an inherent inability of the thyroid gland to produce a sufficient amount of thyroid hormone. About 95% of overt hypothyroidism is primary. Iodine deficiency is the most common cause of primary hypothyroidism. The second most common cause is referred to as “post-theraputic hypothyroidism” due to surgery or radiation therapy for hyperthyroidism. However, primary hypothyroidism can also result from genetic defects, inhibition by drugs or chemicals, cancer, and iodine deficiency or excess.
In any case, the loss of functional tissue leads to a decrease production of TH to which the pituitary responds with an increased production of TSH which increases the synthesis of thyroglobulin, which may lead to thyroid enlargement and goiter results. Laboratory tests reveal elevated TSH with decreasing levels of TH reflective of the severity of the hypothyroidism. Maintenance of T3 levels until the late stages of hypothyroidism is accomplished by both increased secretion of T3 by the thyroid and increased conversion of T4 to T3 in the peripheral tissues.
Secondary hypothyroidism is due to inadequate stimulation of a normal thyroid gland by TSH from the pituitary. Most commonly, this is the result of pituitary tumors (or their treatment) or trauma but can also occur at the level of the hypothalamus. Lab tests will reveal very low TSH levels along with low levels of TH.
Cellular hypothyroidism is a third, less common. Symptoms of hormone deprivation result from a disorder in the peripheral tissues that reduce their responsiveness to TH (TH resistance) or that inactivate the hormone. Lab tests will reveal normal TSH and hormones but there will be low functional thyroid activity (low BMR, low temp)
Clinical symptoms: The characteristic sign of severe, chronic hypothyroidism is myxedema. Myxedema is the result of the build-up of a protein-mucopolysaccharide complex that binds water and produces a non-pitting edema especially around the eyes, hands and feet. It also causes a thickening of the tongue and mucous membranes of the laryngeal and pharyngeal area causing hoarseness and slurred speech.
The symptoms of hypothyroidism usually have an insidious onset and the patient may be unaware of them for years before reaching the stage of myxedema.
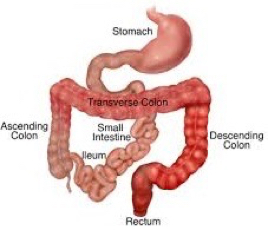
Other Signs and Symptoms: Decreased levels of thyroid hormone leads to a general decrease in the metabolism of fats, proteins and carbohydrates and often result in weight gain, dyslipidemia and an increased risk of cardiovascular disease. Dry skin and hair, brittle nails and significant hair loss are common, and along with a poor tolerance to cold may be some of the first symptoms. Loss of libido, menstrual abnormalities, constipation, muscle weakness and joint stiffness are predominant features although depression, weakness and fatigue are usual.
Difficulty in losing weight is a common complaint of people with an underactive thyroid. Successful weight loss is usually a multi-step process, that includes the following steps:
Optimize Thyroid Treatment: For many patients, to lose weight, it’s not enough to have normal thyroid levels or in the reference range. They need to be optimal. That means a TSH typically below 2.0, Free T4 and T3 in the upper end of the reference range, and lower Reverse T3.
Optimize Blood Sugar: Your fasting glucose level should be balanced.
Balance Hormones: If sex hormones (estrogen, progesterone, testosterone), and adrenal hormones (cortisol, DHEA) are out of balance, this can make weight loss more difficult. Menopause as well as estrogen dominance, can make weight loss more difficult. Lack of testosterone in men and women can make it harder to build muscle. Adrenal imbalance can make you tired, less responsive to thyroid treatment, and less able to lose weight. Evaluating these hormones, and resolving imbalances may be a key step in helping you in your weight loss effort.
Optimize Thyroid Treatment: For many patients, to lose weight, it’s not enough to have normal thyroid levels or in the refence range. They need to be optimal. That means a TSH typically below 2.0, Free T4 and T3 in the upper end of the reference range, and lower Reverse T3.
Optimize Blood Sugar: Your fasting glucose level should be balanced.
Balance Hormones: If sex hormones (estrogen, progesterone, testosterone), and adrenal hormones (Cortisol, DHEA) are out of balance, this can make weight loss more difficult. Menopause as well as estrogen dominance, can make weight loss more difficult. Lack of testosterone in men and women can make it harder to build muscle. Adrenal imbalance can make you tired, less responsive to thyroid treatment, and less able to lose weight. Evaluating these hormones, and resolving imbalances may be a key step in helping you in your weight loss effort.
Food Selection: Eating two to three meals a day, no snacks, and avoiding food after 8 p.m. seem to help balance hunger hormones and blood sugar, and promote fat burning.
Iodine Deficiency: Iodine is a building block for thyroid hormone. Care should be taken so as to not deprive of iodine in daily diet. The best way to include iodine in your diet is with iodine-rich foods – seaweed, shrimp, dried prunes, lobster, cranberries – or use an iodine rich salt.
Goitrogens: Avoid excessive intake of goitrogens. Goitrogens are foods that can induce iodine deficiency by combining with iodine and making it unavailable for use by the thyroid. Foods such as broccoli, cabbage, cauliflower, Brussels sprouts, turnips, walnuts, almonds and soy are considered goitrogenic. Cooking usually neutralizes the goitrogens in these foods.
Nutrition for Hypothyroidism: Protein, Selenium, Magnesium, Iodine, Zinc, vitamin B-12, vitamin B2, vitamin A, vitamin D and vitamin C are important for thyroid function. Make sure your diet has enough of these nutrients or supplements for these vitamins are advisable.
Physical activity: Encourage routine exercise. Exercise stimulates thyroid hormone synthesis, tissue sensitivity and decreases stress, which can interfere with the conversion to active T3.
Also, one should aim to sleep seven or more hours per night as lack of sleep contributes to weight gain and makes weight loss more difficult.