There are few events in everyone’s life that rival the significance — and the joy — of childbirth. The person you’re bringing into the world will become so important to you that you’ll do anything to nurture and protect him or her. You want to do all, you can to help ensure a healthy pregnancy and a wonderful beginning to your child’s life. So you think you want to be a mom — at least sometime shortly. Nutrition during pregnancy also plays an important role to give birth to a healthy child in future parenthood.
How exciting! Having a child is a wonderful experience that will enrich your life forever. But the decision to have a child shouldn’t be taken lightly. Parenthood is a lot of work, and the best way to approach it is by preparing yourself.
About Pregnancy
Pregnancy, also known as gestation, is when one or more offspring develops inside a woman. The term pregnancy is used to describe the period in which a fetus develops inside a woman’s womb or uterus. Pregnancy usually lasts about 40 weeks or just 9 months, as measured from the last menstrual period to delivery. There are three segments of pregnancy, called trimesters. Prenatal care improves pregnancy outcomes. Proper nutrition care helps to have a healthy child.

A woman prepares herself to meet the nutritional demands by increasing her own body fat deposits during pregnancy. Nutrition and lifestyle before and during pregnancy, lactation, infancy, and early childhood have shown long-term effects on the health of the child. This includes the risk of common non-communicable diseases such as obesity, diabetes, and cardiovascular disease. There are other diseases such as an increased risk of adverse pregnancy outcomes including low birth weight, preeclampsia, pre-term birth, and neurodevelopment problems such as fetal alcohol spectrum disorder. This phenomenon is known as “Early metabolic programming of long-term health and disease” or “Developmental origins of adult health and disease”.
Nutritional Status during pregnancy
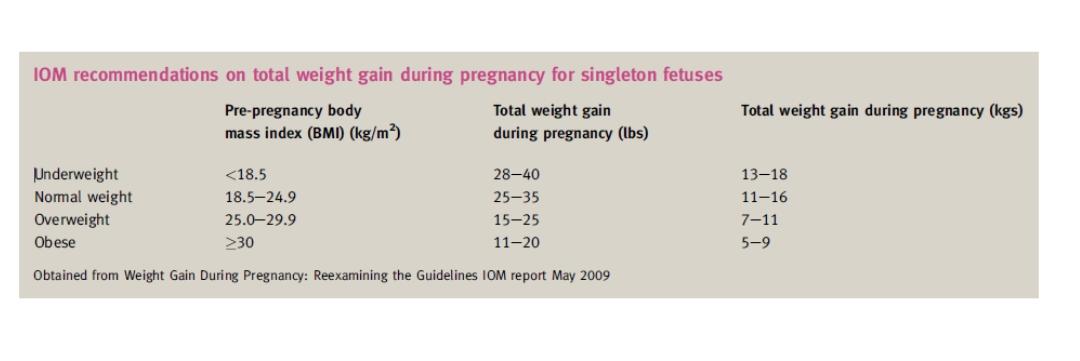
The additional nutritional consumption of a pregnant mother during pregnancy is met by a combination of physiological events, affect maternal nutrient utilization, fatal nutrient transfer, and increased dietary intakes. The physiological changes complicate the interpretation of nutritional status measures in pregnancy. The body composition of the mother in the peri-conceptional period affects pregnancy weight gain. So the new revised weight-gain recommendations continue to be based on maternal body mass index (BMI) at conception.
The adverse effects of consuming an inadequate amount of vitamins and minerals during pregnancy have a long–term effects on deficiencies or their role in specific adverse pregnancy outcomes. Estrogens synthesis is increased from early pregnancy, and its functions include altering carbohydrate and lipid metabolism, increasing the rate of maternal bone turnover.
Nutritional Intake During Pregnancy
The requirements for selected nutrients increase appreciably during pregnancy. The recommended intakes for the following nutrients are >25% higher than the amounts of nutrients that are recommended for non-pregnant women. The nutrition that supposes to consume during pregnancy is protein, α-linolenic acid, iodine, iron, zinc, folate, niacin, riboflavin, thiamin, and vitamin B6. The needs for protein, iron, folate, and vitamin B6 are about 50% higher. Good food sources of these nutrients are grains, dark green or orange vegetables, and the meat, beans, and nuts groups. You also need additional energy to meet the requirements for moving a heavier body, the rise in metabolic rate, and tissue deposition.

Approximately 340–450 kcal should be consumed in the second and third trimesters, respectively. There is a requirement for increased nutrients. The same food pattern recommended for non-pregnant women can also be recommended to pregnant women if the food pattern meets Recommended Daily Allowances (RDA) for all nutrients. The shortfall in iron and vitamin E can be provided by any vitamin-mineral supplement supplying at least 10 mg iron and 9 mg vitamin E.
Healthy eating habits for pregnant mother
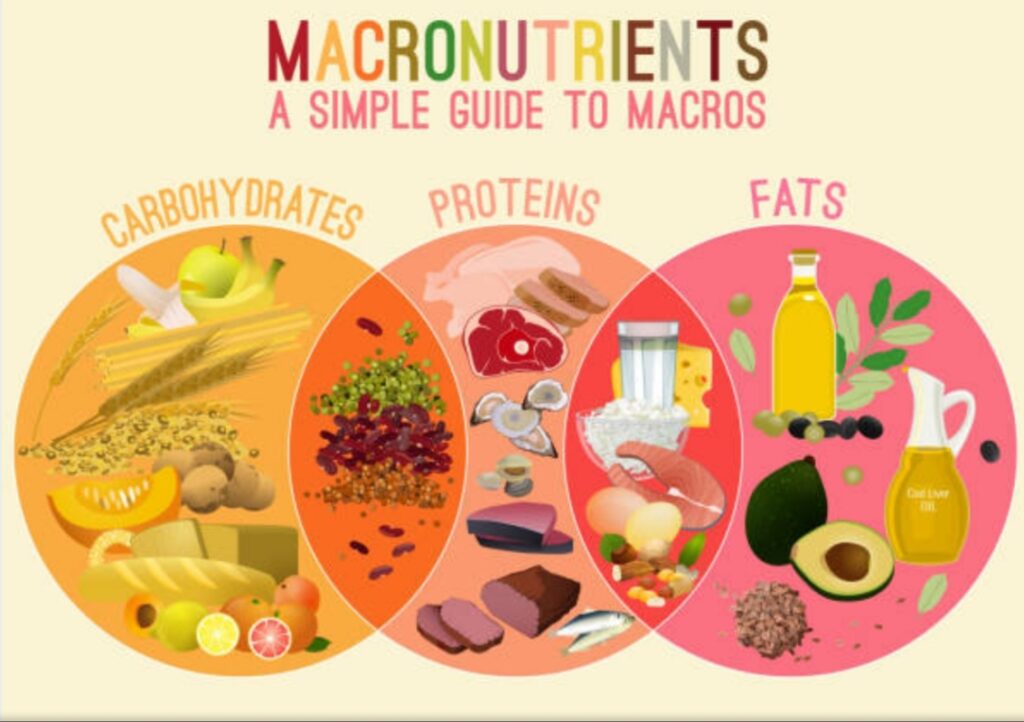
A healthy balanced diet during pregnancy is essential to support optimal growth and development of the fetus and the physiological changes. During pregnancy include consuming optimal amounts of energy as well as macro and micronutrients, achieving appropriate weight gain, adhering to general and pregnancy-specific food safety recommendations. Try to avoid ingestion of harmful substances. The protein, fat, minerals, and vitamins deposited in fetal and maternal tissues come from increased maternal food intake.
The dietary recommendations for pregnant women are to meet their increased caloric and nutrient needs. Additional recommendations include increasing water intake and avoiding foods associated with food-borne illnesses. Should avoid undercooked fish and meat, raw eggs, unpasteurized products, and raw sprouts. Good nutrition is the most important requirement of a mother during pregnancy. Effects of a Poor Diet result in premature birth, low birth weight babies, Feeble, weak babies. A pregnant woman should choose nutrient-dense foods- consume 300 extra calories per day. Eat not more than 12 ounces of low-mercury fish weekly.

No calorie restriction should be there in pregnancy nutrition. Recommendations focus on achieving and maintaining a healthy weight during pregnancy by basing meals on starchy foods (whole grain if possible), eating fibre rich foods, and consuming at least five portions a day of fruit and vegetables. Avoid food that is high in fat and sugar (including fried, some drinks, and confectionery). It is advisable for a pregnant woman to eat breakfast and watch portion sizes and how often they are eating.
Low-fat dairy foods for a source of calcium are encouraged with a daily intake of protein in the form of lean meat, two portions of fish a week (one of which should be oily) or lentils, beans and tofu.
Nutrient requirements during pregnancy
Micronutrients
Energy
The amount of energy required varies greatly among women because of differences in weight and fat gain and energy expenditure. Excessive weight gain in pregnancy tends to cause excessive weight retention postpartum. Exclusive breastfeeding for at least 6 months reduces the risk of long-term retention of this weight.
Carbohydrates
Carbohydrates are the main substrate for fetal growth, fueling maternal and fetal organ function, and biosynthesis. Maternal and fetal brain functions use glucose from carbohydrates as their preferred source of energy with glucose providing at least 75% of fetal energy requirements. An adequate carbohydrate intake will require for cell synthesis.
A low glycaemic index (GI) suggests slower rates of digestion and absorption of a food’s carbohydrate, potentially relating to a lower insulin demand. It is therefore a modifiable macronutrient in the management of diabetes mellitus (gestational, type 1 and type 2).
Protein
Protein forms the building blocks for both structural and functional components of cells. Requirements are highest during the second and third trimesters due to extra development and growth of both maternal and fetal tissue. Plasma concentrations of most amino acids are higher in fetal circulation. Over 15 different amino acid transporters mediate their transport against a concentration gradient.
An additional RDA of 925 g of protein deposits in the mother and fetus, of which 8 g/day are needed during the second and 17 g/day during the third trimester. The total RDA is 1.1 g/kg/ day or + 25 g/day additional protein.
Fat
There are no specific recommendations for fats in pregnancy, apart from following normal dietary guidelines. Fats intake should be 25 to 35 percent of daily calories. Those calories should come from healthy fats, such as avocados and other dry fruits. Foods with unhealthy fats, including French fries and other fast food, should be avoided. It is not recommended for pregnant women to have a very low-fat diet, since it will be hard to meet the needs of essential fatty acids and fat-soluble vitamins.
Fatty acids are important during pregnancy because they support the baby’s brain and eye development. The brain depends on omega-3 and omega-6 fatty acids. Found in salmon and sunflower or safflower oil, for function, structure, and growth. Fats can also help the placenta grow and may help to prevent premature birth and low birth weight. Essential polyunsaturated fatty acids (PUFAs), which must be consumed in the diet, are found mainly in seed oils, the major sources are egg yolk and lean meat. DHA is found in meat and fatty fish.
Fibre
Food rich in fibre affects the postprandial insulin response by influencing the accessibility of carbohydrates and nutrients to digestive enzymes thus delaying their absorption. It supports maternal digestive health, providing bulk to stool and absorbing water to aid transit time. This is especially beneficial as progesterone levels in pregnancy can result in constipation by increasing the relaxation of intestinal smooth muscle.
Micronutrients

Pregnancy nutrition requires certain essential nutrients, supplied only under special conditions, such as stress, illness, or aging. The daily requirements of the nutrients for nonpregnant women change with the onset of pregnancy. Taking a daily supplement or multivitamin helps to meet many nutritional needs during pregnancy. The RDA of nearly all vitamins and minerals increases during pregnancy.
Vitamin A
Excessive supplementation with retinol or the analog isotretinoin will help to treat severe cystic acne. Ingestion of large amounts of retinol is associated with birth defects including abnormalities of the central nervous system, craniofacial and cardiovascular defects, and thymus malformations. The first trimester is most critical as the malformations are from cranial neural crest cells.
Vitamin D
The upper safe limit is 3000 μ g daily for women of reproductive age and in pregnancy. In pregnant and non – pregnant individuals the serum concentration of 25 – hydroxyvitamin D. The main circulating form of the vitamin, is a good indicator of tissue stores of vitamin D. It crosses the placenta and covert to the active form, 1,25 – dihydroxyvitamin D, by the neonate. The placenta synthesizes 1,25 – dihydroxyvitamin D; maternal serum levels are more
Calcium
Calcium is available to the fetus by the substantial increase in the efficiency of maternal calcium absorption starting early in pregnancy. It is carried across the placenta by active transport involving calcium-binding protein and 1,25 – dihydroxyvitamin D. There is little need for additional dietary calcium during pregnancy, and calcium supplements do not improve maternal bone calcium or infant bone in the first year of life, even when maternal intakes are very low. Recommended intakes are 1000 mg/day, the same as for non – pregnant women.
Sodium
The sodium intake should be normal during pregnancy to support the large prenatal expansion of tissues and fluids. Don’t restrict your sodium intake.
Iron
Helps red blood cells deliver oxygen to your baby. Sources include lean red meat, dried beans, peas, and iron-fortified cereals. During pregnancy, you need 28 mg daily, which can be found in most prenatal vitamin supplements. Women who do not have enough iron stored in their bodies before pregnancy may develop anemia. Pregnant women need extra iron in the form of an iron supplement. Your intake of iron should be on an additional 6 mg iron per day during pregnancy. Iron retention by the fetus (300 mg), deposited in the placenta (60 mg), used for the synthesis of additional maternal red blood cells (450 mg), lost in blood during delivery (200 mg) and retained by the mother’s increased red cell mass after parturition (200 mg).
Folate
Folate, also known as folic acid, plays an important part in reducing the risk of neural tube defects. Folic acid is a B vitamin, known as folate, require to meet nutrition during pregnancy. Before pregnancy and during the first 12 weeks of pregnancy, you need 0.4 milligrams (or 400 micrograms) of folic acid daily to reduce the risk of neural tube defects. All women of childbearing age should take a multivitamin supplement containing 0.4 milligrams of folic acid a day.
Women who need 4 milligrams should take folic acid as a separate supplement, not as part of a multivitamin. These are major birth defects that affect the baby’s brain and spinal cord, such as Spina bifida and anencephaly. The American College of Obstetrics and Gynecology (ACOG) recommends 600 to 800 mg of folate. Sources include liver, nuts, dried beans and lentils, eggs, nuts and peanut butter, dark green and leafy vegetables.
Common questions have always been asked by future parents
If a woman is a Vegetarian, what will be her nutritional intake during pregnancy?
A pregnant woman consuming vegetarian diets needs careful nutritional assessment. The vegetarian diet determines the nutrient deficiencies with increased risk. Most pregnant women consuming milk and eggs can meet the increased nutrient needs of pregnancy. You should carefully monitor the Iron Status. Low pre-pregnancy weight and less than optimal weight gain are common problems for vegans. High-calorie foods such as nuts, nut butter, wheat germ, avocados, dried fruit, coconut, honey, and salad dressings may be needed. If you are a vegetarian, you will need to plan your meals with care to ensure you get enough protein. You will probably need to take supplements, especially iron, vitamin B12, and vitamin D.
Vegan diets will require careful planning to consume adequate protein from complementary plant proteins. An alternate source of Vitamin B12 and calcium will require in a vegan diet.
Can being overweight or obese affect pregnancy?
Overweight and obese women are at increased risk of several pregnancy problems. Nutrition during pregnancy plays an important role for overweight and obese pregnant mothers. These problems include gestational diabetes, high blood pressure, preeclampsia, and cesarean delivery. Babies of overweight and obese mothers also are at greater risk such as congenital abnormalities, macrosomia with a possible birth injury, and childhood obesity. If your BMI is 30 or greater. The recommended weight gain is between 11 pounds and 20 pounds during pregnancy. A modest weight loss during pregnancy may be recommended for you if your BMI is 40 or greater.
Can consuming caffeine be harmful during pregnancy?
Moderate caffeine intake (200 milligrams per day—the amount in approximately two 8-ounce cups of brewed coffee) does not appear to lead to miscarriage or preterm birth. It is not clear whether caffeine increases the risk of having a low birth weight baby.
Excess caffeine can interfere with sleep and contribute to nausea and light-headedness. It also can increase urination and lead to dehydration.
How can I plan meals to get the nutrients that I need during pregnancy?
You should join the program of Foodnwellness. This program gives you a personalized diet plan that includes the kinds of foods in the amounts that you need to eat for each trimester of pregnancy.
How Foodnwellness helps during this phase?
Nutrition during pregnancy needs motivation for eating a healthy diet may change relative to the non-pregnant state as women prepare for motherhood and consider the impact of their dietary intake on the baby’s health. Personal values and beliefs about nutrition in pregnancy, advice from health professionals, and physical and physiological changes may interact with behaviors present in the non-pregnant state (e.g., personal preferences, time, money).
Awareness of healthy eating is important during pregnancy, women may lack knowledge of specific dietary recommendations or may not have the skills required to improve their diet. Healthy eating may also be challenging during pregnancy as women face barriers such as food aversions, cravings, nausea, vomiting, tiredness, constipation, hemorrhoids, and heartburn. Women may receive plenty of advice from everywhere but it is worth it when you receive correct knowledge from a panel of health professionals. Foodnwellness will always guide you regarding every issue you face and it will be taken care of by our Dietitians.